After months of gloom, September offered cause for optimism. A review in the scientific journal Nature suggested that a safe vaccine for Sars-CoV-2, the virus causing Covid-19, “might become available in months, rather than years”. The “Superforecasters” at the Good Judgment Project – an American firm that produces impressively accurate predictions of world affairs – put the chances of an approved vaccine being widely available in the US before April 2021 as high as 70 per cent.
But as we entered October, that optimism began to wane. While announcing stricter lockdown measures across large parts of the UK, Boris Johnson engaged in some expectation management, noting that despite “hopeful signs”, a vaccine “cannot be taken for granted”. In early September, the Superforecasters downgraded the pre-April chances of a vaccine, meaning the most likely date was between April and October next year. Although the possibility of a pre-April vaccine has narrowly surpassed the later prediction in recent days, it is still significantly less likely than it was.
The prospect of a year-long wait prompted a strong response from some quarters. On 4 October, three professors unveiled the Great Barrington Declaration, an anti-lockdown statement urging politicians to rethink their current Covid-19 strategies. “Keeping these [lockdown] measures in place until a vaccine is available,” they wrote, “will cause irreparable damage”. They advocate “protecting” older and vulnerable citizens while letting younger people go about their business, hopefully catching Covid-19 as they go and building up natural “herd immunity” to the disease.
The declaration is apparently signed by thousands of scientists and doctors, though since there was no verification of the signatures, a great many came from pranksters, including a “Dr. Person Fakename” and several instances of “Dr. Harold Shipman” (I admit it: I signed the declaration as “Dr. Crippen”). The actual experts shredded the declaration in the Lancet medical journal for failing to define how the “protection” would work, and for providing no plausible means of stopping the young and old from mixing. Attempting herd immunity without a vaccine, the Lancet authors argued, means risking many thousands of lives.
Indeed, the closer the world gets to a vaccine, the more drastically misguided the proponents of “herd immunity” look. So we need to know how seriously we should take the newfound doubts about the vaccine schedule. Why the sudden outbreak of pessimism?
In general, it’s not because the research is untrustworthy. Despite some serious questions about the integrity of the data in a Russian vaccine trial, Covid-19 vaccine studies have so far been admirably free of the biases, errors, and other blunders that have led to the retraction of 36 papers on other aspects of the disease. Vaccine researchers have published their protocols, and transparently noted any last-minute changes. And for what it’s worth, the chief executives of nine pharmaceutical companies have signed a statement saying they’ll stand up to politicians who lean on them to rush their vaccines into production.
[See also: Why a Covid-19 vaccine is only the start]
A more plausible explanation for the pessimism is that multiple Covid-19 vaccine trials have been paused due to unexpected side-effects. This includes the vaccines being developed by AstraZeneca and Oxford University, as well as that by Johnson & Johnson, and it’s concerning: even rare complications will become quite numerous if the target is to vaccinate everyone.
These pauses, however, should be reassuring. The vaccine-makers are doing their very best not to replicate past disasters such as the 1976 flu vaccine, which caused a fourfold increase in the risk of Guillain-Barré Syndrome (a rare, grim autoimmune disorder that attacks muscles). Although the hiatus is frustrating, it’s crucial for ensuring the eventual vaccine is safe.
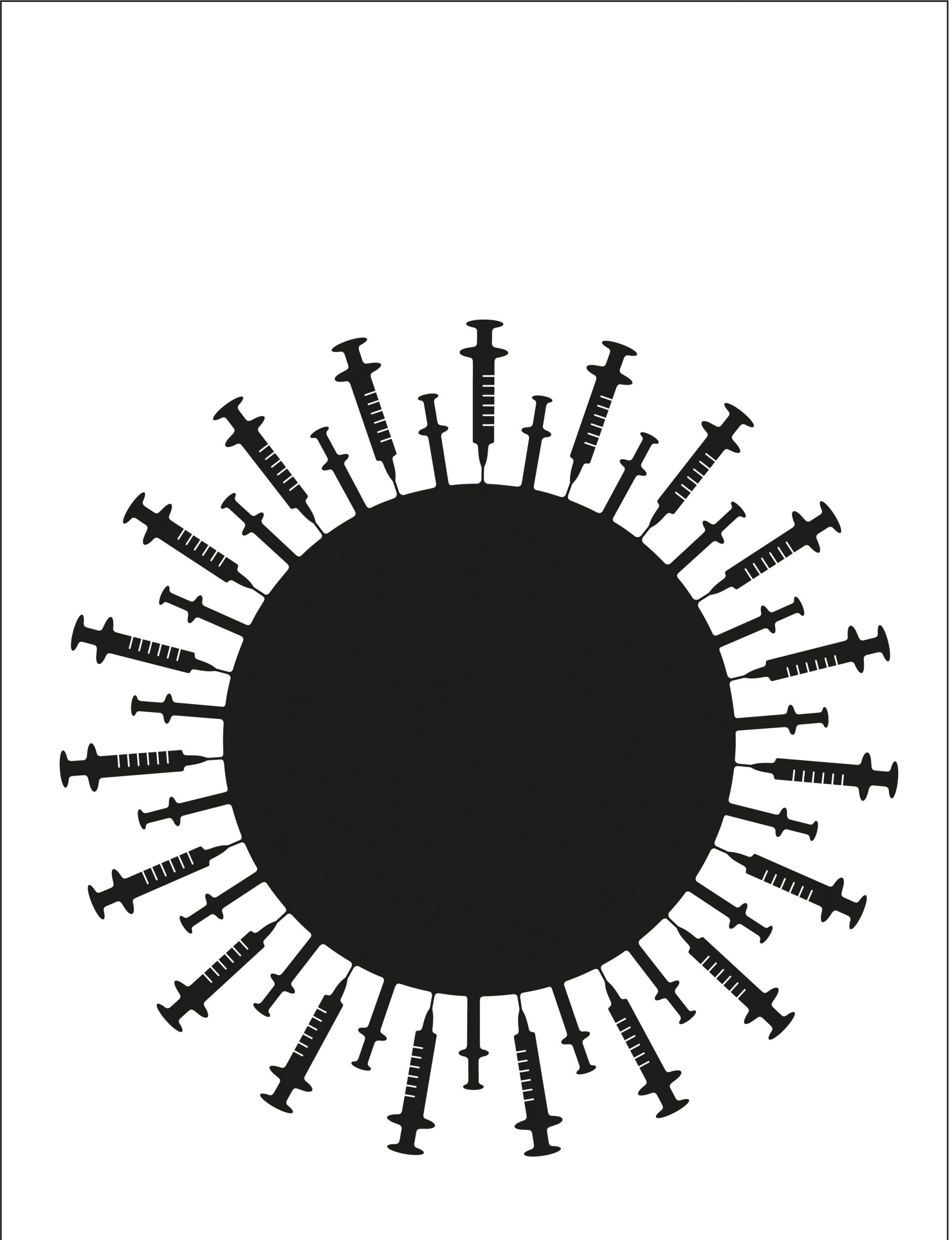
Another cause for added caution about our vaccine predictions is the sheer, Byzantine complexity of the task. Even setting aside the difficulties of running large-scale clinical trials and satisfying regulators, there are countless potential stumbling blocks. It’s possible, for instance, that many of the candidate vaccines will prevent disease in an individual person, but won’t stop them transmitting the virus to others. The logistical task of administering the virus to entire populations is eye-watering, too, replete with challenges such as “have we got enough syringes?” and “how do we keep billions of vaccine vials frozen – especially in countries with under-developed infrastructure?” Finally, one vaccine might not suit all. Different groups – children, pregnant women, people with compromised immune systems – might need entirely different vaccine types.
But therein lies the main reason to feel encouraged: the incredible variety and diversity of the vaccines being tested. We have nearly 200 different vaccine candidates at various stages of development, which work on a variety of different principles – some more traditional, such as those that contain a live, attenuated virus, and some more experimental, such as those based on DNA. These different methods have various pros and cons; should the vaccines that are currently in late-stage trials disappoint, a whole cast of alternative candidates is waiting in the wings. The logistics are improving, too: companies and governments are working to improve the supply chain and inventing new ways of transporting frozen vaccines to where they’re needed.
Despite the recent fall in confidence, the world is still on course for a vaccine sooner rather than later. Unlike so many other aspects of the scientific and policy response to Covid-19, vaccine development has gone extraordinarily well so far. The smart money isn’t on the fatalistic strategy of herd immunity – a false promise in any case. The progress of vaccines shows science rising admirably to an almost unimaginably difficult task – and should give us plenty of reasons for optimism.
[See also: Why Sweden did not pursue “herd immunity” against Covid-19]
Stuart Ritchie is a psychologist at King’s College London and the author of Science Fictions: How Fraud, Bias, Negligence and Hype Undermine the Search for Truth






