If health outcomes are to improve, and cost less, the NHS needs to work much more closely with industry – as a strategic partner, not just a provider of equipment.
This was the argument presented by Jeroen Tas, chief executive of health-care informatics, solutions and services at Philips, speaking at the NHS Health and Care Innovation Expo in September.
“The future health of millions of children, the sustainability of the NHS and the economic prosperity of Britain all now depend on a radical upgrade in prevention and public health,” Tas said. “More broadly, we need to engage with communities and citizens in new ways, involving them directly in decisions about the future of health and care services. To achieve this, over the next five years and beyond, the NHS will increasingly need to dissolve traditional boundaries and rethink the models of care delivery.”
He is not alone in his thinking. The NHS also recognises that the status quo cannot be maintained. In its Five Year Forward View, it outlines the challenges our health service faces, which include a “mismatch between resources and patient needs of nearly £30bn”, “unacceptable variations of care provided”, and the need to address widening gaps in health and well-being, care and quality, and funding and efficiency.
“One response to these challenges would be to attempt to muddle through the next few years, relying on short-term expedients to preserve services and standards. Our view is that this is not a sustainable strategy . . .” reads the document, adding that the identification of, and joint working with, similar health communities forms an important element of the new approach.
New ways of working have to include new ways of working with industry.
Take the role of digital technologies within the NHS. Despite the internet playing such a big role throughout most of our lives – be that for banking, shopping or entertainment – only 2 per cent of patient interactions with the NHS take place online. As the Internet of Things starts to connect- people’s worlds even more, this is going to drive similar demands within health care, and while the NHS may be one of the best health systems in the world, it is not a tech company. If the power of digital is to be realised in health and well-being, new alliances will need to be formed between NHS organisations, medical technology companies and cloud platforms.
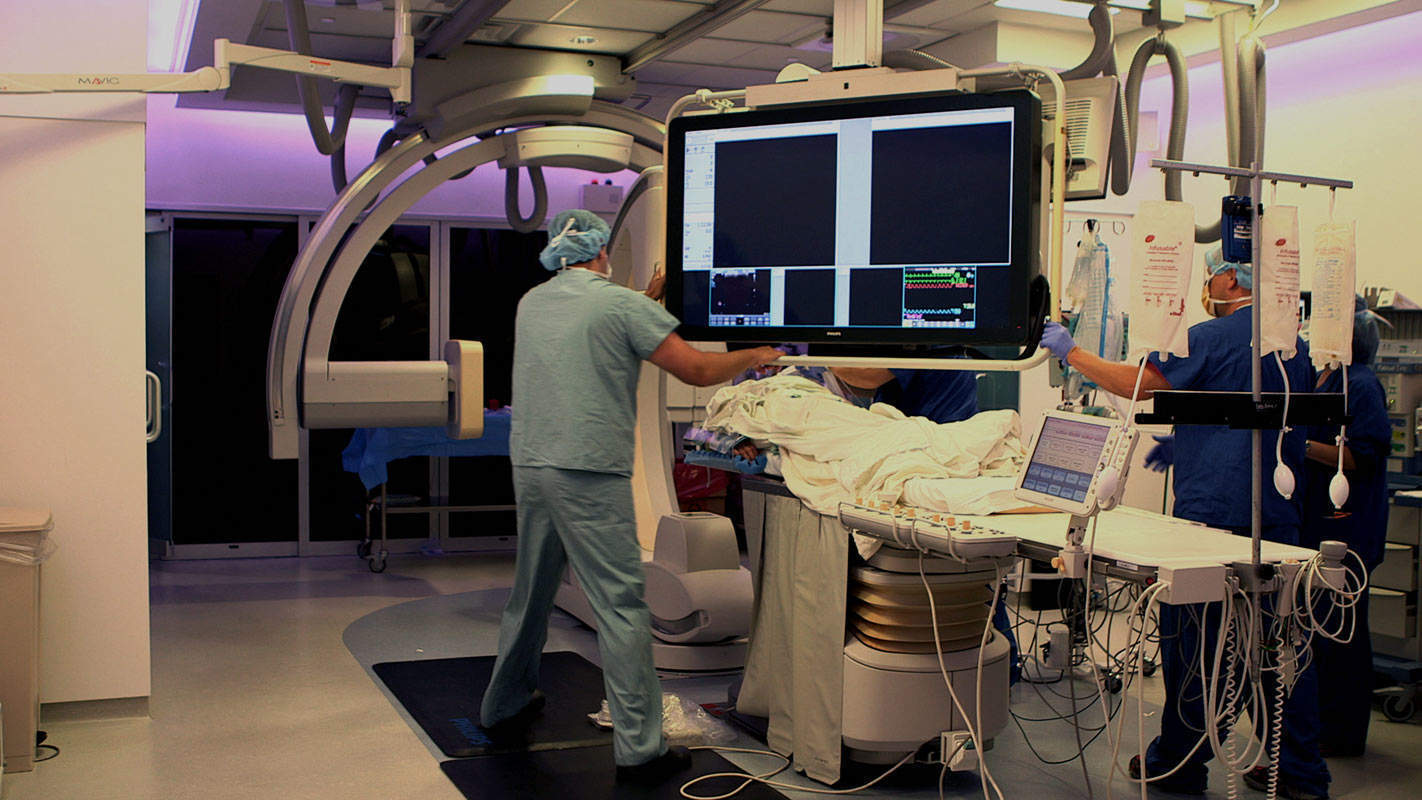
These kinds of partnerships and collaborations are already starting to come to fruition. Philips, for example, has recently launched Digital HealthSuite, in partnership with Salesforce, which combines customer engagement with leading medical technology and informatics for people with long-term -conditions such as diabetes and chronic obstructive pulmonary disease (COPD). By providing these patients with the technology to record their personal data, and combining this with clinical data, it is possible to enable more informed care decisions, driving a reduction in emergency admissions, and thereby reducing pressure on the health service. “Complex algorithms attuned to patients’ vital signs and profiles can identify a serious situation and ensure timely intervention,” Tas explains.
The NHS has also made a worldwide call for innovators to partner with local health and care systems in trialling new technologies, digital services and other innovations, such as equipping patients with wearable tech or helping clinical staff better manage long-term conditions.
“The digital revolution is transforming our lives in many sectors but the health sector is lagging in reaping the potential rewards. The test bed is a hugely important opportunity to bring together the needs of health care and the creative energy of industry to speed the implementation of digital technologies for patient benefit and to promote economic growth,” says Sir Mark Walport, the Government Chief Scientific Adviser.
Elsewhere, procurement processes are also beginning to change, says George MacGinnis, health-care expert at PA Consulting, a management consultancy with a specialism in health care. “Typically the NHS decides it wants something and goes to market to buy it,” MacGinnis says. “It is now beginning to understand the different additional value offering – is there risk that can be shared, for example?”
MacGinnis refers to parallels with the Ministry of Defence, which changed the nature of the deals it was brokering with aircraft manufacturers. “They didn’t just buy the aircraft, they bought having a number of aircraft ready to fly. The NHS is starting to work in a similar way – a telehealth company might not just offer a piece of equipment but could also be responsible for maintaining and servicing the equipment. They may agree to train NHS staff in how to use it; and they might even offer to run the associated clinical service for them,” he explains.
However, there are a number of barriers to adoption of new ways of working. The propositions on offer from industry need to become scalable, reliable and open, and the user experience needs to be harmonised. Meanwhile, both the public and health-care professionals need to become more familiar with the new arrangements. Central to this is trust.
“Consumers, patients and professionals alike will need the right motivation, reassurance and mindsets to adopt these new solutions,” Tas says. “The companies that know how to offer tailored, cutting-edge solutions, combined with meaningful advice and trustworthiness, will be the winners and become trusted advisers in health.”
Richard Phillips, the director of public policy at the Association of British Healthcare Industries (ABHI), agrees it is about trust. And he adds: “Medical technology companies are driven by the need to save and improve lives. I don’t think industry should be shy about the fact that it makes returns, as that allows it to do other things [that the NHS isn’t always able to do], such as R&D.”
Regulation, of course, has a role to play in helping engender this trust. So, too, does accountability. “Change needs to be led by clinicians and not industry, and the NHS needs to ensure it is transparent when declaring the value it gets from services,” MacGinnis says.
Transitioning from a system that is organised around acute events to one that supports monitoring and remote care with multidisciplinary teams requires redesign. New technology will drive how services are delivered, which in turn will dictate where and how medical professionals work, and the knowledge and skills they need. Ensuring the workforce has the flexibility to adapt to different working environments will be critical to effective partnership working, particularly considering the speed at which new iterations of tech are developed.
Meanwhile, NHS funding structures are another barrier to be overcome. Currently, both innovation and budgets are siloed and annualised.
“Annualised budgets mean that people are under pressure to deliver savings in one year when it can take longer than this. This means that sometimes activities can make sense for a ward or department but can be illogical for the organisation as a whole,” says ABHI’s Phillips. “Paper towels offer the simplest example. For example, cheap paper towels may appear to save money but because they are thin, people have to use more of them and it ends up costing much more in both volume needed and waste removal. We want to see more joined-up thinking between risk and investment.”
Equally, if new reimbursement models are to be explored, there are many conversations that must be had about how the health outcomes analysis takes place.
“While paying companies based on their results is a great goal to aim for, the clinical outcomes might not happen for many years, and when they do, they can be difficult to measure accurately,” MacGinnis says.
This is where data helps. The information collected through connected devices, for example, is providing much deeper insights into both individual and population health trends that could begin to provide the data on clinical outcomes that will facilitate more payment by results.
Of course, technology alone is not going to bring about change. It requires leadership, buy-in throughout the health service and among the public, and it requires innovation.
“We see exciting and sometimes turbulent times ahead for the health-care industry,” Tas reflects. “I am sure the result will be a step change in the quality and cost of care.”
This article is part of a thought-provoking series on living health, brought to you by the New Statesman in association with Philips, which looks at how technology, innovation and big data are helping to improve your health and our health-care system.






