The National Health Service runs on three things: public money, staff good will and jargon. Of these three, only the latter never seems in danger of exhaustion.
The NHS is festooned with jargon. Swimming in it. NICE, QIPP, QUALY, AfC; PCTs, CCGs, F1s, and F2s. I spent two years writing for the weekly trade newspaper GP, during which I became something of an expert in the nGMS contract for GPs, plus of course MPIG and QOF. (Obviously one can’t truly understand the nGMS contract without understanding MPIG.) Getting to grips with that remains one of the most intellectually challenging things I’ve ever done, yet it’s been of no use whatsoever in the wider world. It’s the public policy equivalent of learning Klingon.
There is, however, one bit of NHS jargon that more of us probably should understand. “Reconfiguration” means, in essence, changing where patients have to go to get different bits of healthcare. And the reason it’s worth getting your head round is that it lies at the root of so much of so many of the rows about changes to NHS services.
That includes, one suspects, this week’s row about clause 119 of the of the care bill, which would allow administrators appointed by the health secretary to chop bits off hospitals, without bothering with the trifling matter of public consultation. Jeremy Hunt’s motivations for wanting such power may indeed be exactly as sinister as everyone seems to expect. Then again, it’s just plausible that the clause is simply a recognition of the fact that, at present, reconfiguration is simultaneously a) vital, and b) damn near impossible because no one ever wants to close anything. Hunt’s latest wheeze may be nothing more dodgy than an attempt to fix a dysfunctional system.
To explain why, we need to explain why reconfiguration is necessary in the first place. Demand for healthcare is rising, thanks to an ageing population, but it’s also changing: where once healthcare was something people received in short sharp bursts when sick, it’ll increasingly be something that a significant chunk of the population need access to all the time.
Hospitals aren’t really set up to cope with this ongoing, low-level care, which most people would much rather have closer to their home anyway. They’re also expensive (big buildings, big overheads). And, as medicine has become more specialised, a consensus has developed that you’re better off being treated in a big hospital full of experts rather than a small one without any. If you’re admitted to your local district general with a suspected case of Elledge’s Disease on a Friday, but the consultant who specialises in it only visits on a Wednesday, then that’s five days in which you’re going to have to make do with the care of junior doctors and nurses who know relatively little about the disease. All that time, you’re stuck in a hospital bed, and costing the NHS money. (Oh, and you might die. Nasty condition, Elledge’s disease.)
So – for a long time everyone’s wanted to make the health service less dependent on the traditional model of a hospital in every town. Instead of the bog standard district general that does everything, as much healthcare as possible would be provided by smaller community centres (polyclinics, extended GP practices, that sort of thing). Meanwhile, the hardcore stuff would be handled by a smaller number of really big hospitals, and networks of centres that specialise in specific conditions (stroke, cancer, and so on). All this should save money. It’d be more convenient. And it could also, though this bit’s more contentious, provide better care.
But reconfiguration brings its own problems, too. While this brave new world would see a lot of patients treated closer to their homes, some, especially those from rural areas, would have to travel further. That probably means longer life-or-death dashes in ambulances with sirens blaring; at the very least, it means fewer visits from friends and family.
More than that, though, it means closing hospitals, or at least bits of them, and that is bloody hard to do. There’s nothing that excites a local newspaper as much as a campaign to save the local A&E department; nor is there anything more likely to turn a loyal front bencher into a shouty rebel. (Don’t believe me? Here’s William Hague protesting against NHS cuts in his constituency.)
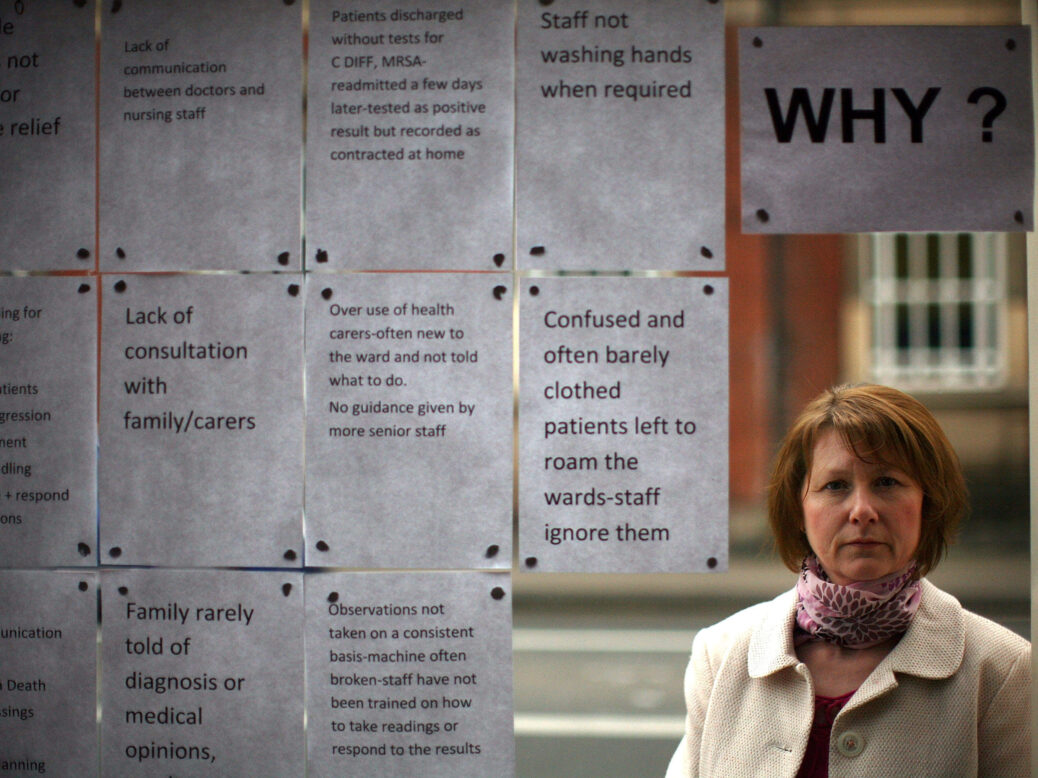
So while policy wonks and politicians generally support reconfiguration in the abstract, once you start talking about closing specific things, and people realise they’re going to lose doctors/services/jobs/votes, it tends to evaporate. And, to the layperson, defending an NHS facility from closure because it’s a vital public service, and doing so for sentimental or political reasons, tend to look exactly the same.
The problem is, if the NHS can’t reduce the money it spends on expensive district generals, it won’t be able to afford all the shiny new stuff that’s meant to replace them. Closing important services for financial reasons is stupid. But closing expensive things we don’t need so that we can spend the money on new things that we do isn’t. I’m not pretending it’s easy to know which is which; but if the health service is to improve we need to at least be open to the possibility that redundant services exist.
As time goes on the demands on the health service are going to change, and to do some things better it’ll need to stop doing other things badly. Reconfiguration matters, and it means that your local A&E might have to close. Shouldn’t we have an honest conversation about that?






